Self-Care for Busy People: Simple Strategies for Taking Care of Your Mental Health
Self Care is often something last on our minds. Here are some tips on how to incorporate self-care into your busy life.
Self Care is often something last on our minds. Here are some tips on how to incorporate self-care into your busy life.
Living with a partner who has ADHD can be difficult at times, especially if you don’t know how to properly support them through your relationship while still focusing on yourself. Take a look at some tips for supporting a partner with ADHD and how to work through their ADHD symptoms together.
Working from home is great if you remember to keep your mental health in mind! Here are five essential tips for working from home
Claudia Hernandez is in the spotlight sharing what brought her to the therapy profession, what challenges her clients face and more.
Dana Norden is in the spotlight again talking about challenges her clients face and her favorite self-care activities.
Joslyn Meissner is in the spotlight again sharing what challenges her clients face, her favorite self-care activities and more.
Adriane Barton is back in the spotlight sharing what challenges her clients face, what a therapy session is like with her, and her self-care activities.
Here’s a little secret about my own relationship. My husband regularly goes on hiking trips with people he has met on the Internet (often women!). Oh, and I don’t go on said trips with him and often have never met the people he goes with. He really enjoys hiking/backpacking and well, I don’t as much. I went on a few hiking trips with him and I just didn’t have that great of a time. This is his hobby and passion. I’ve got other hobbies that he has no interest in as well.
Guess what? I consider my relationship pretty rock solid and wonderful.
How can that be, you may ask? Some questions/remarks I have heard throughout the years… “Why in the world do you let your husband meet people let alone other women and spend all day with them in the woods?” “Aren’t you afraid of something happening?!” “What kind of husband would go on a hiking trip without his wife?” And oh so much more….
We live in a culture where we are taught not to rely on others for emotional support and yet see relationship red flags when two people do hobbies independent from one another.
The answer, to put it simply at first, is no, I am not worried because I trust him and I do not want to deprive him of something he is truly passionate about (nature, hiking/backpacking, mountains etc.). I do worry about him when he is hiking though safety-wise!
The more complicated answer has to do with what Mary Ainsworth, a developmental psychologist, called a secure base. She did an experiment studying attachment with infants and mothers called the Strange Situation Test. Basically, a child is put into a room with toys and the mother leaves the room and comes back. The child with a secure attachment style, while upset that the mother left, is able to be soothed by her, and then uses her as a secure base and is able to go out and explore the toys with confidence while glancing at her/his mother. The child knows that she needs her mother, her mother is available.
As adults, we are put into ‘strange situations’ every day, whether they are at work, with friends, or even when our husbands are in another state hiking with people we don’t know. Ok, maybe the last one is just me… Having a secure base as an adult is having someone who, in your time of need, 100% has your back and is supportive of you. It’s someone whom you can depend on and vice versa. As adults, we are capable of knowing that our partners are there for us emotionally and psychologically even if they are not close in proximity. If your partner makes you feel safe and is able to reassure you during hard times, you are free to focus your attention on other things that make your life more meaningful, such as hiking.
Early on in our relationship, there were many times where my husband stood up for me, gave me pep talks, and had my back and I for him. We created this security early on, but it wasn’t always smooth sailing (more on that in later posts). My husband is my secure base and I am his. This type of relationship may look very independent from the outside. He’s off hiking on the weekends, I’m back in Chicago. On the contrary, we are actually very dependent on one another. *gasp* He is the first person I turn to if I need advice on just about anything. He opens up to me about his work stress. We are very emotionally close. So how can we be emotionally close but physically apart for a good portion of the weekends in the summer when he is off hiking?
This is what attachment theorists call the “dependency paradox” meaning the more dependent you are on someone during hard times and they are available to meet your needs, the more independent you become. Think of the kid who stands up to the class bully because they know their friends have their back either way or the husband who applies for a job promotion out of state and rocks the interview knowing he has his wife’s full support and that they will make things work no matter what happens.
The saying “if you love someone, let them go, if they return, they were always yours” comes to mind, but I’d tweak it a little bit. I would say “if you love someone to the point that you can depend on him or her to have your back and support you and likewise you for them, let them go. Do your own thing, they’ll be back and they’ll tell you how much fun they had and how they wished you were there too.” You’ll both probably feel more satisfied with your relationship and your lives.
I was walking home yesterday and I heard a man on his phone say “My back is bothering me again, so I thought I’d call and get it checked out.” I can assume he was talking to his doctor or chiropractor. This got me thinking about how his conversation would have been different had he been calling a therapist (or any mental health professional). Would he feel comfortable having the same conversation talking about his anxiety, (“My anxiety is acting up again, so I thought I’d call and get it checked out”) in a public place with a handful of people able to hear his conversation? Maybe, but most likely not.
The initial phone calls I receive from clients are ones with hushed voices or sometimes tears. Most people don’t even call, they opt for e-mailing instead. This got me thinking or should I say hoping that one day people will be able to freely have that conversation with a therapist just like they would a back doctor without the shame or stigma attached.
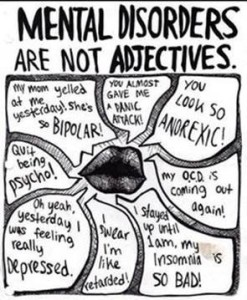
One of the most memorable moments in my training as a therapist was when I was an intern during the summer between my junior and senior years of college. I was working in a partial hospitalization program at a local hospital. While I was observing a group psychotherapy session, all of a sudden the therapist slammed his hand down on the table and said (in a very loud voice) “NO! You are NOT bipolar. Bipolar disorder is something you have, NOT something you are and since you have it you can manage it. The fact that you have bipolar disorder does not and should not define who you are as a person.” That moment really stuck with me and still does to this day.
So often, we use mental illness as an adjective or a word that describes a noun (usually ourselves or another person) when in fact if you look up “anxiety” in the dictionary it states “noun 1. a feeling of worry, nervousness, or unease, typically about an imminent event or something with an uncertain outcome.” or “depression” as “noun 1. the state of feeling sad.” Sure, depressed is technically an adjective. But I hope you see my point here. When did society start defining themselves by their current mental state and making it more of a permanent attribute when it really is not? People already define themselves by their current careers, much to their detriment. I can only imagine the harm defining yourself by your current mental state. It leaves very little room for flexibility (career-wise or mental-state wise!) to even think of yourself in any other way.
I like to do my part in separating clients from their mental illness (making it a noun and not an adjective) and I correct them when they say “I am depressed” by saying “You have depression” or “You are experiencing anxiety” rather than “I am anxious.” I also give this little word game as homework to clients so that they can start the shift and start seeing their current mental state as temporary and not something that has to define them. Hopefully people will soon reference mental illness like they do physical illness “I have a backache” “I have a cold” “I have anxiety.” I have never heard anyone say “I am a backache.”
Hopefully this post leaves you with the take-home that one’s current mental state does not have to define him or her. It’s as simple as switching a few words around in your lexicon to begin making that change.
One of the best TED talks I was ever introduced to was one by Brene Brown called “The Power of Vulnerability.” I’ve read a few of her books, but I still like to watch the TED talk every now and then to remind myself how important vulnerability is within the therapeutic setting.
I often have clients say to me in session “I’m sorry I was so emotional” or “I’m sorry I cried the whole time.” It’s interesting to me that clients feel the need to apologize for their vulnerability during session. I can definitely see why they do this. Most people were raised not to express vulnerable emotions, weaknesses, and flaws. Having to do just that while in therapy for one hour each week or so can be incredibly intimidating! I remember I had one client who said he needed to “take time” after our sessions because he was not used to telling anyone, let alone someone he didn’t really know, about his unpleasant emotions and flaws.
I am always careful not to placate or invalidate a client’s vulnerability by saying “it’s ok.” Instead, I try to thank them for trusting me enough to be vulnerable in session because that is what I need to see in order for clients to make changes in their life. As a therapist, it is often difficult for me to sit with my clients when they are so vulnerable. In a way, I empathize so much, that I start to feel vulnerable myself. This is a process for me and for every therapist.
I believe that once you can have a vulnerable conversation, one where you express and sit with your true and unpleasant feelings/thoughts, in the therapeutic setting, you can start to be vulnerable in your every day life. State dependent learning anyone? Take that client I mentioned earlier, he was exercising his “vulnerability muscle” if you will. Soon, he was able to have more emotion-focused conversations with his wife, where he would admit his insecurities about their marriage. This brought them closer and wouldn’t have happened had he not practiced and become more comfortable with being vulnerable.
My challenge to you, is to make yourself emotionally vulnerable to someone once a week to start flexing your “vulnerability muscle.” For me, this is usually admitting to someone that I do not know the answer and will have to look it up, asking for directions, or admitting I was not fully listening to a friend or family member when they were speaking. Each time I do something like this, I become more comfortable with being emotionally vulnerable and I would hope this makes me more equipped to sit with vulnerability in the therapy room. My hope is that it would also allow my clients to be more vulnerable with me in session. After all, if you cannot be vulnerable with your therapist, who is un-biased and non-judgmental, with whom can you be?

Please note that we require a 24-hour notice if you decide to cancel your appointment. Call or email to cancel or reschedule at least 24 hours before your scheduled appointment in order to avoid charges. We will do our best to accommodate you and appreciate your cooperation. Thank you.
